- 1 - Who is it for
- 2 - How to take
- 3 - Ingredients
- 4 - Frequently Asked Questions
Probiotics for women
ProbioGea Donna (ProbioGea for Women) is Salugea’s 100% natural food supplement that provides a selection of probiotics designed to specifically support women's intimate health.
It can be used as a prevention or in the acute stages when a prompt response is needed. ProbioGea innovative formulation helps counteract the most common discomforts affecting women’s intimates, often due to unhealthy lifestyle or habits - such as the use of harsh vaginal cleansers, unbalanced diet, stress, etc. – or to physiological hormone variations usually occurring during the menstrual cycle, pregnancy and menopause.
The probiotic strains in ProbioGea Donna can also help maintain a healthy balance of the bacterial vaginal flora after an antibiotic therapy.
How does ProbioGea Donna work and why is it different from any other women’s probiotic supplements available on the market today?
For maximum efficacy, we have selected probiotics that normally belong to the vaginal flora, combined them with a functionally tested Patented Probiotic Complex, and Lactoferrin a substance of proven efficacy in terms of support for the woman’s intimate well-being.*
The synergistic action developed by the 100% natural ingredients helps maintain a healthy balance of bacteria in the vulvovaginal area over time and counteracts the effects of the imbalance of the vaginal bacterial flora, especially if they tend to repeat frequently.*
Besides, ProbioGea Donna for vulvovaginal health is practical and easy-to-use as it is taken orally (by mouth). In fact, the active ingredients are contained in acid-resistant capsules designed to protect probiotics from the harsh acidic environment of the stomach thus ensuring that they are released in the intestines and uro-vaginal tract where they can be absorbed effectively.
Finally, ProbioGea does not contain colourings, preservatives or artificial sweeteners.
*Please refer to the “Scientific Insights” section where all the clinical and scientific studies are listed.
Who is ProbioGea Donna for?
ProbioGea Donna formulation is for women who:
- wish to naturally sustain their vulvovaginal well-being over time by supporting also the physiological balance of the bacterial flora of the intestines,
- experience vaginal flora imbalance frequently or from time to time, due to stress-related factors, unhealthy diet, menstrual cycle or antibiotic therapies,
- are going through pregnancy or menopause and wish to protect themselves against the effects of unbalanced vaginal flora caused by hormonal changes,
- are looking for a practical, easy-to-use natural remedy.
*Please refer to the “Scientific Insights” section where all the clinical and scientific studies are listed.
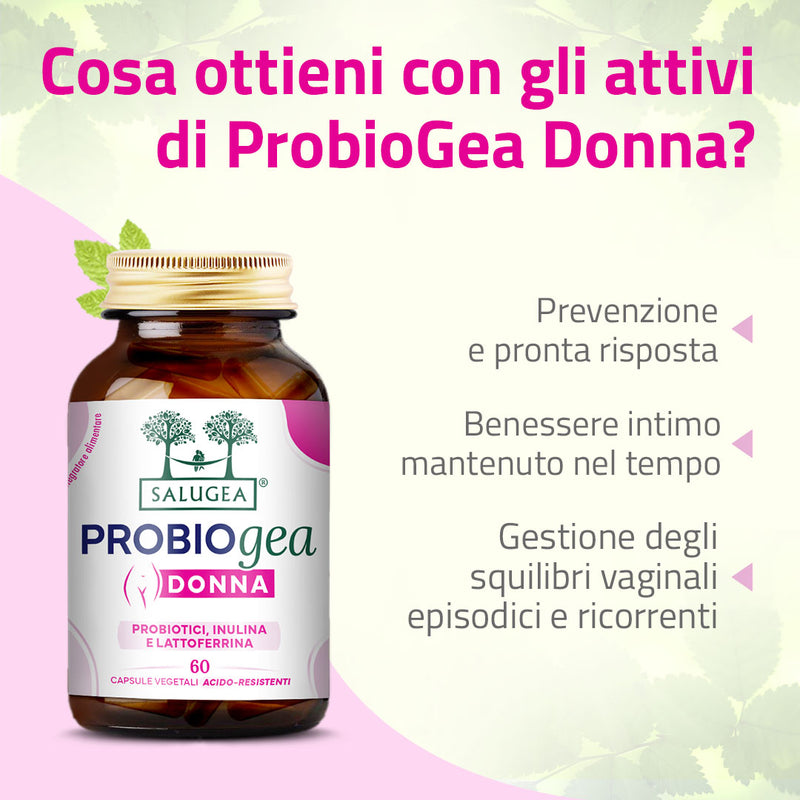
What benefits will you obtain from ProbioGea Donna active ingredients?
- You sustain your vulvovaginal well-being, for prevention and when a prompt response is needed.
- You recover the balance of your vaginal flora when unhealthy lifestyle or habits, hormonal changes or antibiotic therapies negatively affect it.
- You counteract the effects the vaginal flora imbalance as soon as they appear, also when they tend to repeat frequently (recurrent).*
- You supplement your body with probiotics that are naturally present in a healthy vaginal environment.
- You supplement your body with a patented probiotic complex.
- You supplement your body also with L
- You take your supplement orally (by mouth) as it comes in practical acid-resistant capsules.
* Please refer to the “Scientific Insights” section where all the clinical and scientific studies are listed.
Make your choice consciously!
The preservation of the product is crucial: inadequate preservation can lead to the inactivation of live cells.
Hence, make sure you choose probiotics that:
- are stored in pharmaceutical-grade brown glass bottles (not in plastic or blister packs),
- are contained in acid-resistant capsules, which allow the cells to reach the gut alive and vital.
The PROBIOGEA line of probiotics is the result of years of research by the Salugea Research and Development Team.
Our probiotics are all:
- formulated with specific strains, supported by clinical studies that confirm their efficacy at the declared dosages,
- enclosed in acid-resistant capsules,
- stored in pharmaceutical-grade brown glass bottles,
- featuring innovative formulations based on patented probiotic complexes,
- offering a wide variety of probiotics.
Be careful not to be misled! A large number of live cells or strains does not necessarily mean greater benefit!
- If not properly preserved, you will actually consume far fewer than stated,
- your gut may have difficulty tolerating them.
Why is ProbioGea Donna different from any other women’s probiotics?
- It is stored in practical and durable pharmaceutical-grade brown glass bottles. Glass is the only material that can guarantee the quality and safety of the product over time, and it is environmentally friendly!
- It is 100% natural.
- It supports the balance of the vaginal flora with a synergistic formulation: a patented ingredient of lactobacilli and bifidobacteria, combined with other probiotics typically and naturally present in a balanced vaginal microbiota, and Lactoferrin.*
- It offers multiple strains of probiotics to effectively balance vaginal flora and maintain well-being over time.*
- It delivers probiotics in acid-resistant capsules, protecting them during the gastric transit and ensuring they arrive alive and vital in both the intestinal and vaginal environments.
- Its active ingredients all come from 100% natural sources (not made in a lab).
- It has an innovative formulation.
- It is gluten-free.
*Please refer to the “Scientific Insights” section where all the clinical and scientific studies are listed.
How does ProbioGea donna, the probiotic supplement for women, work?
Patented Probiotic Complex: Lactiplantibacillus plantarum PBS067, Lacticaseibacillus rhamnosus LRH020, Bifidobacterium animalis subsp. lactis BL050.
According to studies*, this complex:
- acts against agents that may settle and develop in the vaginal environment, causing imbalances,
- promotes the balance of vaginal flora even with oral intake and maintains results over time – it is also useful in cases of recurrent imbalances,
- supports vaginal health during menopause,
- has a strong antioxidant effect (and consequently also an anti-inflammatory action).
Lactobacillus crispatus, vaginal lactobacillus.
Lactobacillus crispatus is a “good” bacterium of the female urogenital tract that plays a crucial role in protecting the vagina from agents that cause imbalances in its bacterial flora.*
This probiotic, typical of a healthy vaginal microbiota, supports intimate well-being even when taken orally: it can beneficially colonise the intestines and subsequently also the vagina.*
Lactobacillus fermentum, to enhance synergy.
Lactobacillus fermentum is a symbiotic (i.e., "good") bacterium of the human gut, also playing a key role in controlling and inhibiting agents that cause vaginal imbalances.*
It has been shown that the combination of L. fermentum and Lactobacillus rhamnosus (a lactobacillus present in the patented probiotic complex) is particularly beneficial: together, these two strains strongly restore balance in the vaginal environment while reducing the presence of harmful bacteria and imbalance-causing yeasts.*
Lactoferrin, for an additional synergistic action
Lactoferrin, recognized for its immune system benefits, also provides support for vulvovaginal well-being.
Studies have shown that the combination of lactobacilli and lactoferrin, when used alongside antibiotic treatments for vaginal infections, helps reduce symptoms and recurrence, offering these benefits even to pregnant women.*
Inulin from chicory
Inulin is a soluble prebiotic fiber recognized for its significant benefits to the gut and its physiological functions, as it helps develop “good” bacterial strains*, which indirectly supports intimate health by promoting the beneficial colonisation of the vaginal environment.
The inulin in ProbioGea Donna comes from chicory and has a very low content of free sugars such as fructose, glucose, and sucrose (below 10%).
*Please refer to the “Scientific Insights” section where all the clinical and scientific studies are listed.
HOW TO TAKE
For maximum benefits, we suggest that you take 2 capsules of ProbioGea Donna a day.
- Mid-morning, away from main meals*: 1 capsule of ProbioGea Donna
- Mid-afternoon, away from main meals*: 1 capsule of ProbioGea Donna.
*Away from main meals means at least one hour before or after your meals.
Keep the product at room temperature, in a cool and dry place, away from moisture, heat, and direct sunlight.
Once opened:
- do not discard the security seal under the cap and reuse it each time you close the bottle,
- make sure to close the bottle tightly after each use,
- do not store the bottle in the refrigerator,
- consume possibly within 60 days of opening.
Duration of the treatment with ProbioGea Donna
After a short time, you will see the results and feel the benefits. We recommend that you continue the treatment for at least three months to reach the best results and keep them over time. Remember to suspend the treatment for 2 to 3 days every 30 days of intake. The suspension is suggested, not compulsory, as it helps keep the ingredients effectiveness high.
At the end of the three-month treatment with 2 capsules, you can just repeat it (for a stronger action) or switch to 1 capsule a day for a few months to extend the duration of the benefits.
During the treatment or at the end of it, please contact us! We care for you and would be very pleased to know how you got on and how you feel. Our Team of experts (Biologists, Nutritionists, Chemists and Naturopathic Doctors) will be happy to help you take the next steps to maintain over time the results you have achieved.
Please Note. As we are all different (and unique!), the dosage can be set according to your specific needs and requirements. Just give us a call or write to us for any kind of information or advice you may require. Our experts shall remain at your fullest disposal ;)
Taken alone, ProbioGea Donna is extremely effective and gives you excellent results. Yet, for a stronger action, you may want to combine it with:
- Colonsan Formula Potenziata, a mix of specific plant extracts to support digestion and bowel transit especially in case of “gas in the belly”.
- Intestinum Forte, with natural active ingredients that help promote regular intestinal functions and balance in hypersensitive/hyper-reactive intestines.
- Sanuril Formula Potenziata, with plant extracts beneficial for the urinary tract, also when imbalances of the gut microbiota allow for "bad" bacteria to move from the vagina to the bladder, and the other way round.
- Pausanorm Forte, a next-generation, soy-free formulation designed to alleviate all the menopause and pre-menopause discomforts, including vaginal dryness.
Warning
Supplements cannot be considered as a replacement for a balanced diet and a healthy lifestyle. Keep out of reach of children under the age of three. Do not exceed the recommended daily dosage. The expiry date refers to the product intact, stored in a cool and dry place, away from heat, humidity and direct sunlight.
INGREDIENTS
Chicory Inulin, Acid-resistant capsule (coating agent: hydroxypropylmethylcellulose; gelling agent: gellan gum), Limosilactobacillus fermentum LF58, Lactiplantibacillus plantarum PBS067, Lacticaseibacillus rhamnosus LRH020, Bifidobacterium animalis subsp. lactis BL050, Lactobacillus crispatus LCR6, Lactoferrin (whey protein), Anti-caking agents: Silicon dioxide, Vegetable magnesium stearate. Probiotics are supported on maltodextrin and corn starch.
Nutritional Values
|
AVERAGE AMOUNT OF NUTRIENTS PER DAILY INTAKE (2 Capsules) |
|
|
Lactiplantibacillus plantarum PBS067 |
1 Bn CFU |
|
Lacticaseibacillus rhamnosus LRH020 |
1 Bn CFU |
|
Bifidobacterium lactis BL050 |
1 Bn CFU |
|
Limosilactobacillus fermentum LF58 |
2 Bn CFU |
|
Lactobacillus crispatus LCR6 |
1 Bn CFU |
|
Lactoferrin |
50 mg |
|
UFC: Colony-Forming Unit |
|
SCIENTIFIC INSIGHTS
The connection between intimates discomfort and vaginal pH.
Itching, burning, foul-smelling discharge... Throughout their lives, almost all women experience, to varying degrees, vaginal discomforts like these, which might be the sign of inflammation: vaginitis. When vaginal inflammation has an infectious origin, it is referred to as vaginosis.
Vaginitis and vaginosis are originally linked to a variation in vaginal pH. Under normal conditions, the pH is particularly acidic (4-4.5), which inherently reduces the risk of developing infections.
However, there are factors that can cause fluctuations in pH, triggering mechanisms that ultimately lead to the onset of the most common vaginal discomforts.
Causes and consequences of vaginal pH fluctuations
Among the main triggering factors, we can mention:
- physiological hormonal variations related to the menstrual cycle, pregnancy, or menopause,
- the use of irritating products, from “aggressive” intimate cleansers to detergents used for washing clothes,
- a diet excessively rich in sugars, cheeses, baked goods, and fermented beverages, such as beer and alcoholic drinks in general,
- alterations of the gut and urinary tract microbiota,
- prolonged conditions of stress or fatigue that can weaken the vaginal immune defences,
- wearing tight clothing or synthetic underwear.
When these factors lead to significant changes in vaginal pH, pathogenic agents are given the green light. In simple terms, they colonise the vaginal bacterial flora thus causing more or less significant imbalances that manifest through specific symptoms. The most common include:
- white-grayish vaginal discharge (leukorrhea), rather watery and foul-smelling,
- itching of varying intensity,
- burning during urination,
- pain during sexual intercourse.
Pathogens responsible for vaginal infections
The pathogens that most often cause vaginal infections include:
- bacteria, such as Gardnerella vaginalis and Escherichia coli,
- fungi, such as Candida,
- protozoa, such as Trichomonas vaginalis.
There are also many cases where a specific cause cannot be identified. In a review of studies published between 1966 and 20031, it was found that for about 30% of symptomatic cases, a precise diagnosis could not be made.
Sometimes they come back!
Another interesting fact concerns recurrent conditions, such as vaginitis or vaginosis, which tend to repeat with some frequency. It has been estimated that in Italy, 75% of women have experienced at least one episode of vulvovaginal candidiasis in their lifetime, and 40-45% have had two or more episodes.1
How to fight against vaginosis and vaginitis
Therapeutic strategies often involve the use of antibiotics, both orally and vaginally (in the form of suppositories, creams, or gels). They are generally effective during the acute stage, but their intake has to be evaluated with a doctor especially in case of recurrence, as there is a risk of developing antibiotic resistance through repeated antibiotic treatments.
The real key to prevention.
- Maintain proper intimate hygiene. Consult your gynecologist or pharmacist about the most suitable products and methods for keeping the vaginal area clean. You might be advised not to use internal vaginal douches, change hygienic towels frequently during menstruation, and limit the use of tampons and liners.
- Wear breathable cotton underwear and, in general, choose clothing that is not too tight.
- Pay attention to your diet. One key piece of advice: avoid excessive consumption of foods high in refined sugars and yeasts.
- Protect yourself during "risky" sexual intercourse by using barrier methods, such as condoms.
- Use specific probiotics to support your vaginal bacterial flora, which helps prevent the growth of pathogens, while also supporting the gut microbiome.
Speaking of probiotics, let’s have a look at some studies conducted on the probiotics we have selected for the formulation of ProbioGea Donna.
Scientific Studies
A patented mix of probiotics: Lactiplantibacillus plantarum PBS067, Lacticaseibacillus rhamnosus LRH020, Bifidobacterium animalis subsp. lactis BL050
Presti I, D’Orazio G, Labra M, et al. Evaluation of the probiotic properties of new Lactobacillus and Bifidobacterium strains and their in vitro effect. Appl Microbiol Biotechnol. 2015 Jul;99(13):5613-26. doi: 10.1007/s00253-015-6482-8. Epub 2015 Mar 7. PMID: 25744647.
Various in vitro tests have recognized this patented mix as effective in countering the settlement and proliferation of pathogenic germs, such as Escherichia coli, and in providing a steric competition (essentially, pathogens do not have enough space to adhere and proliferate). Additionally, a co-aggregation mechanism with urogenital pathogens has been observed, meaning that probiotics tend to cluster pathogenic urogenital bacteria together, thereby inhibiting their functionality. This effect has been demonstrated against Candida albicans, Escherichia coli, Gardnerella vaginalis, Candida glabrata, Trichomonas vaginalis, and Neisseria gonorrhoeae (see Evaluation of Antimicrobial, Antiadhesive and Co-Aggregation Activity of a Multi-Strain Probiotic Composition against Different Urogenital Pathogens doi: 10.3390/ijms24021323).
All these actions allow the probiotic complex to slow down tissue inflammatory states, help activate the immune response by increasing the release of IL-4 cytokines (IL-4 stimulates immune defences) and provide a significantly greater synergistic antioxidant potential compared to individual strains (meaning it exerts an antioxidant effect, and consequently, an anti-inflammatory effect as well). Additionally, the probiotic complex protects the cellular vitality of the epithelium after induced stress (research has shown that the epithelial tissue lining the vaginal environment exhibits increased vitality once the "good" bacterial film from the patented formulation is established).
Mezzasalma V, Manfrini E, Ferri E, et al. Orally administered multispecies probiotic formulations to prevent uro-genital infections: a randomized placebo-controlled pilot study. Arch Gynecol Obstet. 2017 Jan;295(1):163-172. doi: 10.1007/s00404-016-4235-2. Epub 2016 Nov 9. Erratum in: Arch Gynecol Obstet. 2017 Feb;295(2):527. PMID: 27826653.
This clinical study investigated the efficacy of the patented multi-strain probiotic formulation used, administered orally, to prevent urogenital infections. The study involved 40 healthy women, divided into a test group and a placebo group. The treatment group took the probiotic mix for 14 days, while the other group received an inert product. The specific probiotic mix demonstrated its ability to reach and colonise the vagina through oral intake, with a significant increase in the vaginal concentrations of the various strains in the test group compared to the placebo. Additionally, the vaginal pH levels showed a significant reduction, even during the period when product administration was suspended. This indicates that these patented probiotics, when taken orally, can beneficially colonise the vagina, resulting in a significant and lasting colonization effect.
Murina, Filippo & Vicariotto, Franco. (2019). Evaluation of an Orally Administered Multistrain Probiotic Supplement in Reducing Recurrences Rate of Bacterial Vaginosis: A Clinical and Microbiological Study. Advances in Infectious Diseases. 09. 151-161. 10.4236/aid.2019.93011.
This important clinical study recruited 75 women (aged 18-50) suffering from recurrent bacterial vaginosis. After treatment with the antibiotic metronidazole, the test group received the patented probiotic mix, while the placebo group was given an inert product. The mix of L. plantarum PBS067, L. rhamnosus LRH020, and B. animalis subsp. lactis BL050 provided significant relief from symptoms after the acute treatment and was able to reduce symptom worsening over time, whereas the placebo group experienced symptom aggravation. Moreover, in the group that took the probiotics, the success rate of the antibiotic therapy improved by 24%, and the recurrence rate dropped by 40%. Finally, this mix demonstrated a clear superiority in restoring the vaginal microbiota compared to the placebo group.
Vicariotto F, Malfa P, Viciani E, et al. Efficacy of Lactiplantibacillus plantarum PBS067, Bifidobacterium animalis subsp. lactis BL050, and Lacticaseibacillus rhamnosus LRH020 in the Amelioration of Vaginal Microbiota in Post-Menopausal Women: A Prospective Observational Clinical Trial. Nutrients. 2024 Jan 30;16(3):402. doi: 10.3390/nu16030402. PMID: 38337685; PMCID: PMC10857347.
Due to hormonal deficiencies, vulvovaginal issues (such as intimate dryness, inflammatory states, and an increased tendency for vaginal infections) can intensify during menopause. In this clinical study, 50 healthy postmenopausal women aged between 45 and 65 were given a patented mix of lactobacilli and bifidobacteria for 28 days. The probiotic complex demonstrated up to a 50% improvement in vaginal health for menopausal women (assessed through vaginal elasticity, secretion, mucosal state, integrity, and lubrication) and helped restore a healthy vaginal pH by re-establishing lactobacilli, which inhibit the growth of pathogens. Additionally, there was a significant reduction in inflammatory markers, with results observed within one month that persisted over time. Finally, the analysis of the vaginal microbiota showed that the patented mix promotes an increase in "good" bacteria typical of vaginal flora and reduces the presence of recurring vaginal pathogens such as Streptococcus, Gardnerella, Atopobium, Escherichia, and Shigella.
Lactobacillus crispatus
De Seta F, Campisciano G, Zanotta N, Ricci G, Comar M. The Vaginal Community State Types Microbiome-Immune Network as Key Factor for Bacterial Vaginosis and Aerobic Vaginitis. Front Microbiol. 2019 Oct 30;10:2451. doi: 10.3389/fmicb.2019.02451. PMID: 31736898; PMCID: PMC6831638.
The classification of the vaginal microbiota can be based on the relative abundance of various species of specific lactobacilli, identifying five different microbial communities known as “Community State Types” or CSTs. In this study, women with a CST I microbiota, characterized by the prevalence of Lactobacillus crispatus and a pH of 4, showed the lowest risk of vaginosis or contracting milder infections. While a completely rigorous ranking cannot be established, L. crispatus appears to be the most protective among lactobacilli for the well-being of the vaginal environment.
Mändar R, Sõerunurk G, Štšepetova J, et al. Impact of Lactobacillus crispatus-containing oral and vaginal probiotics on vaginal health: a randomised double-blind placebo controlled clinical trial. Benef Microbes. 2023 Apr 18;14(2):143-152. doi: 10.3920/BM2022.0091. Epub 2023 Mar 1. PMID: 36856121.
This interesting placebo-controlled clinical study tested the use of Lactobacillus crispatus, administered both orally and vaginally, in women with bacterial vaginosis (BV) and vulvovaginal candidiasis (VVC) aged between 18 and 50. The study showed that both oral and vaginal capsules reduced signs and symptoms in patients with BV, with notable improvements in discharge as well as itching/irritation. In patients with VVC, the oral capsules were able to lower the combined score of the two most important symptoms: the amount of discharge and itching/irritation. Notably, the oral treatment with L. crispatus performed comparably for bacterial vaginosis and even better for candidiasis compared to vaginal administration, thus representing an equally effective but more practical and convenient therapeutic method.
Lactobacillus fermentum
Kaur, Baljinder & Balgir, Praveen & Bhartimittu, Dr & Chauhan, Ashish & Kumar, Balvir. (2013). Purification and Physicochemical Characterization of Anti-Gardnerella vaginalis Bacteriocin HV6b Produced by Lactobacillus fermentum Isolate from Human Vaginal Ecosystem. American Journal of Biochemistry and Molecular Biology. 3. 91-100. 10.3923/ajbmb.2013.91.100.
This interesting in vitro study highlighted how Lactobacillus fermentum can metabolise proteins known as bacteriocins, which have a bactericidal effect against Gardnerella vaginalis, the primary bacterium responsible for vaginosis. The study demonstrated that this protein produced by L. fermentum strongly inhibits the growth of G. vaginalis, thereby serving as an important probiotic for women's intimate health.
Reid G, Charbonneau D, Erb J, Kochanowski B, et al. Oral use of Lactobacillus rhamnosus GR-1 and L. fermentum RC-14 significantly alters vaginal flora: randomized, placebo-controlled trial in 64 healthy women. FEMS Immunol Med Microbiol. 2003 Mar 20;35(2):131-4. doi: 10.1016/S0928-8244(02)00465-0. PMID: 12628548.
This placebo-controlled clinical study, conducted on 64 women, investigated the synergistic action between Lactobacillus fermentum and Lactobacillus rhamnosus (also present in the patented probiotic complex) on the vaginal microbiota. Microscopic analysis of vaginal swabs showed that oral administration of L. rhamnosus and L. fermentum achieved significant results in restoring a normal microflora populated by lactobacilli and in reducing coliform bacteria (pathogenic bacteria) and yeasts.
Kang CH, Kim Y, Han SH, Kim JS, Paek NS, So JS. In vitro probiotic properties of vaginal Lactobacillus fermentum MG901 and Lactobacillus plantarum MG989 against Candida albicans. Eur J Obstet Gynecol Reprod Biol. 2018 Sep;228:232-237. doi: 10.1016/j.ejogrb.2018.07.005. Epub 2018 Jul 9. PMID: 30014929.
In another study, the in vitro synergy between Lactobacillus fermentum and Lactobacillus plantarum (a strain present in the probiotic mix) was tested against Candida albicans. The tests revealed that the cells of C. albicans lost their metabolic activity and were ultimately eliminated.
Lactoferrin
Russo R, Karadja E, De Seta F. Evidence-based mixture containing Lactobacillus strains and lactoferrin to prevent recurrent bacterial vaginosis: a double blind, placebo controlled, randomised clinical trial. Benef Microbes. 2019 Feb 8;10(1):19-26. doi: 10.3920/BM2018.0075. Epub 2018 Dec 10. PMID: 30525953.
The aim of this clinical study was to evaluate the efficacy of a probiotic mix, including Lactobacillus acidophilus and Lactobacillus rhamnosus, combined with bovine lactoferrin, as an adjunct therapy to the antibiotic metronidazole in women with recurrent bacterial vaginosis. Forty-eight volunteers with recurrent bacterial vaginosis were divided into a test group and a placebo group. Initially, they received metronidazole as acute treatment, followed by the test product or placebo for 10 days each month for 6 months, starting on the first day of menstruation. The results showed that symptoms (vaginal discharge and itching) and the recurrence rate were significantly reduced by the probiotic mix in combination with lactoferrin. In conclusion, this approach may represent a safe and effective remedy for restoring a healthy vaginal microbiota and preventing recurrences of bacterial vaginosis.
Russo R, Superti F, Karadja E, De Seta F. Randomised clinical trial in women with Recurrent Vulvovaginal Candidiasis: Efficacy of probiotics and lactoferrin as maintenance treatment. Mycoses. 2019 Apr;62(4):328-335. doi: 10.1111/myc.12883. Epub 2019 Feb 20. PMID: 30565745.
Vulvovaginal candidiasis (VVC) is a recurring condition in pregnant women. This study evaluated the efficacy of an oral formulation containing Lactobacillus acidophilus, Lactobacillus rhamnosus, and bovine lactoferrin on the symptoms and recurrence of VVC as an adjunct therapy to topical clotrimazole. Forty-eight pregnant women positive for C. albicans, with symptoms of VVC and a documented history of recurrences, were randomly divided into two groups that received either the probiotic complex or a placebo as adjunct treatment for clotrimazole, following a maintenance cycle of 6 months (1 capsule/day or placebo for 10 consecutive days each month). Symptoms, overall healing rate, and recurrence rate were assessed. After therapy with clotrimazole, a significant improvement in symptoms was observed in both groups. However, only the women treated with probiotics and lactoferrin showed significant improvement in itching and discharge at 3 and 6 months. During the six-month follow-up, recurrences were significantly lower in the intervention group compared to the placebo: 33.3% vs. 91.7% after 3 months and 29.2% vs. 100% after 6 months, indicating a threefold improvement. The results demonstrate that the mixture of lactobacilli in combination with lactoferrin represents a safe and effective adjunct approach to reduce symptoms and recurrences of vulvovaginal candidiasis, even in pregnant women.
Inulin from chicory
Qin YQ, Wang LY, Yang XY, et al. Inulin: properties and health benefits. Food Funct. 2023 Apr 3;14(7):2948-2968. doi: 10.1039/d2fo01096h. PMID: 36876591.
This review of studies focuses on the function of inulin and its health benefits, including its recognized prebiotic activity, which stimulates the growth of beneficial bacteria and contributes to the balance of the gut microbiota. This action indirectly impacts on intimate well-being, as the development of these "good" bacteria in the intestines also promotes subsequent beneficial vaginal colonization.
Hughes RL, Alvarado DA, Swanson KS, Holscher HD. The Prebiotic Potential of Inulin-Type Fructans: A Systematic Review. Adv Nutr. 2022 Mar;13(2):492-529. doi: 10.1093/advances/nmab119. Epub 2023 Feb 10. PMID: 34555168; PMCID: PMC8970830.
This review of studies confirms the beneficial prebiotic function of inulin on the gut microbiota (increased levels of bifidobacteria and lactobacilli) and on the gut barrier. It's important to remember that intestinal health and vaginal health are always closely interconnected.
DISCLAIMER
Our texts are for informational purposes only and should not be considered as indications for diagnosis and treatment of pathological conditions. They cannot replace your physician’s advice.
I nostri testi hanno scopo divulgativo, non vanno intesi come indicazione di diagnosi e cura di stati patologici e non vogliono sostituirsi in alcun modo al parere del Medico.
Cod. Min. Sal.: 179006
I nostri testi hanno scopo divulgativo, non vanno intesi come indicazione di diagnosi e cura di stati patologici e non vogliono sostituirsi in alcun modo al parere del Medico.
ProbioGea Donna
Probiotics for Women
Domande Frequenti sull'integratore
Altre Domande?
Se non hai trovato la risposta alla tua domanda, puoi contattarci: